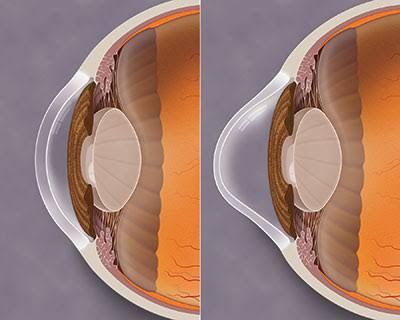
Keratoconus (literally, conical cornea) is a thinning and steepening of the central zone of the cornea, the front surface of the eye. These ‘wonky windows’ cause irregular astigmatism, where the unusual shape of the cornea causes the light to bend as it passes through, resulting in blurred vision. If left untreated, keratoconus can lead to severe vision impairment.
An inherited disorder, keratoconus occurs in about 1 in 800 people. Considered a recessive condition it requires genetic factors to be inherited from both parents. It is exacerbated by eye rubbing. Keratoconus usually becomes apparent between the ages of 10 and 25 years. It is sometimes associated with other conditions such as allergies, infantile eczema, asthma, reduced night vision, double jointed-ness and, in rare instances, with occasional short bouts of chest pain.
Glasses and contact lenses can give good vision and collagen cross linking surgery can be used to slow progression and penetrating keratoplasty may be required to treat severe cases. Collagen crosslinking, which increases the stiffness of the cornea, has been introduced as a treatment with reported success in slowing progression. However, the procedure is only suitable for keratoconus patients at the early stages of disease, and long-term outcomes are not yet known.

In about 85 per-cent of cases of Keratoconus, the condition stabilizes by age 35 years. In the remaining 15 per cent, the condition progresses and vision and tolerance to contact lenses may deteriorate. For members of this group, a corneal graft may be necessary.
A corneal graft or penetrating keratoplasty is an operation in which the thinned area of the cornea is removed and replaced by normal tissue transplanted from a donor cornea. Corneal grafting is used only when all other methods for correcting vision have failed to provide good vision. The success rate for corneal grafts is high, although most will still need to wear contact lenses following the grafting.
Patients require lifelong follow-up and there is a risk of graft failure from immune rejection of the donor tissue, with subsequent grafts having an increased risk of rejection.
Dr Ieuan H. Rees. (Optometrist)
Buck & Todd Optometrist
Located at 103 Alfred Street, Mackay, 4740.