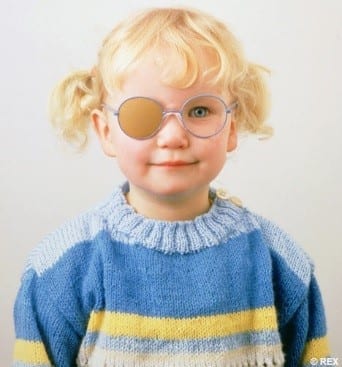
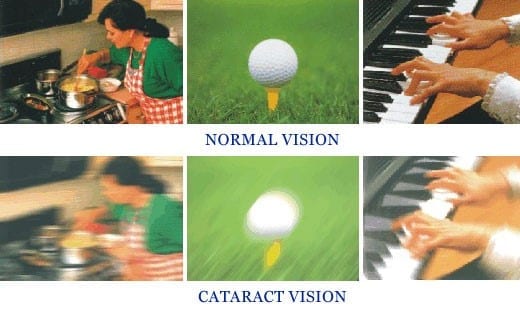
Macular Degeneration impairs a person’s ability to read, recognise faces, drive, and makes it difficult to recognise colours and contrasts.
Commonly affecting people over 50 years of age it is referred to as ‘age-related macular degeneration’ or AMD. There is currently no cure for AMD, and treatment efforts are directed at maintaining useful central vision for as long as possible.
It never causes complete blindness as the surrounding (side) vision remains normal, but it is the leading cause of vision loss in the western world, accounting for almost 50% of all visually impaired cases.
There are two types of AMD: dry (atrophic) and wet (neovascular or exudative). Most AMD starts as the dry type and in 10-20% of individuals, it progresses to the wet type. Age-related macular degeneration is always bilateral (i.e., occurs in both eyes), but does not necessarily progress at the same pace in both eyes. It is therefore possible to experience the wet type in one eye and the dry type in the other.
Macular Degeneration is the leading cause of blindness in Australia and affects central vision.
Dry vs Wet Macular Degeneration
The dry (atrophic) type affects approximately 80-90% of individuals with AMD. It tends to progress more slowly than the wet type, and while there is not—as of yet—an approved treatment or cure most practitioners recommend a healthy diet, cessation of smoking and vitamin supplements to help maintain a healthier macula. In dry age-related macular degeneration, small white or yellowish deposits, called drusen, form beneath the macula causing it to deteriorate or degenerate over time.
The wet/neovascular type affects approximately 10-15% of individuals with age-related macular degeneration, but accounts for approximately 90% of all cases of severe vision loss from the disease.
In wet age-related macular degeneration, abnormal blood vessels under the retina begin to grow toward the macula. Because these new blood vessels are abnormal, they tend to break, bleed, and leak fluid, damaging the macula and causing it to lift up and pull away from its base. This can result in a rapid and severe loss of central vision.
Causes
The causes of AMD are not fully understood however the major risk factor is increasing age. The disease seems to cluster in certain families, suggesting that some are more genetically susceptible than others.
Symptoms
The main symptom of AMD is blurring of the central vision, with many people experiencing difficulty when reading. People also experience blurred, dark, or empty spots, similar to the after effect of looking into a flashbulb. A frequent and important symptom is distortion, straight lines such as door frames or street poles may appear bent or wavy.
Almost all patients with AMD can see well enough to take care of themselves and continue activities that do not require detailed vision.
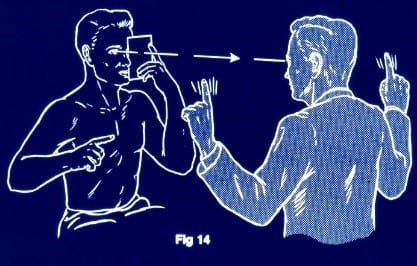
Diagnosis
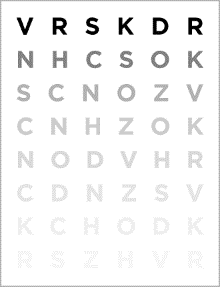
Regular eye examinations are the best way to detect AMD, this should be conducted by an Optometrist. If you experience any of the symptoms above, please make an appointment as soon as possible.
Risk Factors
Research suggests there are things that can be done to reduce the risk of developing AMD, including:
- stop smoking,
- eat a diet rich in fresh fruit and dark green leafy vegetables,
- increase your intake of fish and other omega rich foods,
- supplement your diet with vitamins, minerals and antioxidants,
- protect your eyes from ultraviolet light,
- check your vision regularly with your doctor.
Treatment
There is currently no cure for AMD, and treatment efforts are directed at maintaining useful central vision for as long as possible. Treatment varies depending on the type of AMD and individual characteristics of the condition.
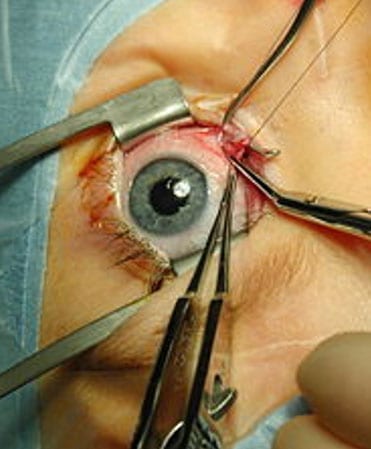
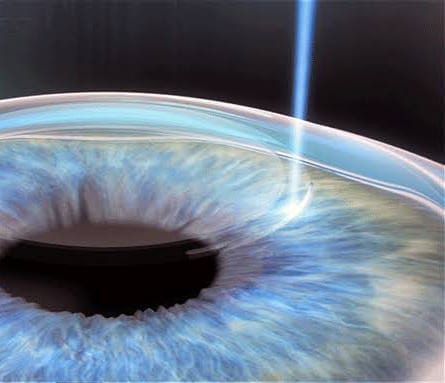
The most common treatment available for wet AMD is injection of Anti-VEGF agents: Ranibizumad (Lucentis), Aflibercept (Eylea) and Bevacizumab (Avastin). These drugs are injected into the vitreous cavity of the eye, reducing leakage from the blood vessels under the retina. Since this is not a cure, the majority of patients receiving these treatments will require life-long therapy at 1-3 monthly intervals.
There are currently no proven treatments to reverse the effects of dry AMD. Some vitamins, minerals and antioxidants ‘may’ slow down the progression of early stage of AMD
For more information see contact the Macular Disease Foundation: http://www.mdfoundation.com.au/
Dr Ieuan H. Rees. (Optometrist)
Buck & Todd Optometrist
Located at 103 Alfred Street, Mackay, 4740.


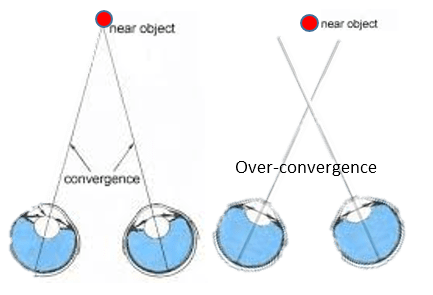
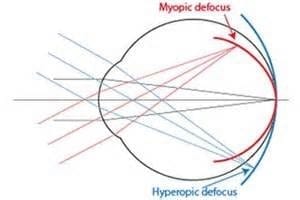
 Daily low dose 0.02-0.05% atropine is reasonably effective (64%) in slowing myopia progression. However even at this minimal concentration, glare sensitivity and need for reading glasses can occur. “WARNING” Long term use of anticholinergic medications has recently been linked to cognitive impairment and earlier onset of dementia.
Daily low dose 0.02-0.05% atropine is reasonably effective (64%) in slowing myopia progression. However even at this minimal concentration, glare sensitivity and need for reading glasses can occur. “WARNING” Long term use of anticholinergic medications has recently been linked to cognitive impairment and earlier onset of dementia.


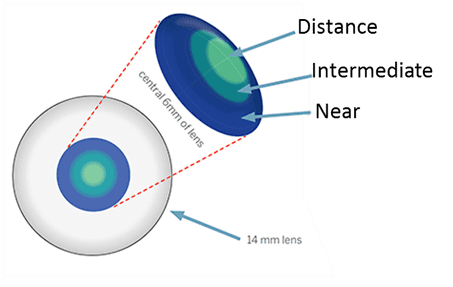


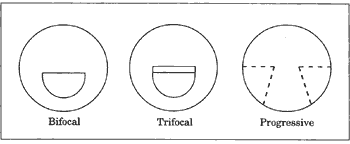
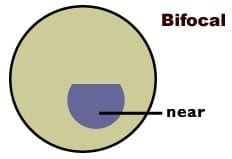 There are two distinct areas to a bifocal lens. In most cases the top portion is used for distance viewing and the lower portion for reading and other close work such as sewing.
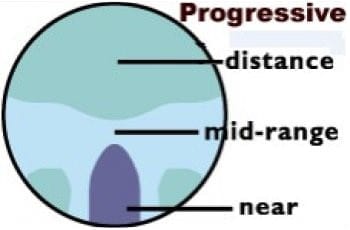
There are two distinct areas to a bifocal lens. In most cases the top portion is used for distance viewing and the lower portion for reading and other close work such as sewing.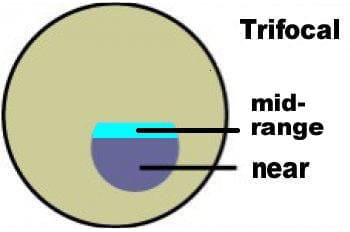 It is important for some people to be able to focus clearly at mid-range between distance and near. For example, Musicians may need to see their instruments close-up and read music at arm’s length while still being able to see the conductor in the distance. Someone with these needs will require trifocals, which give clear vision at three distances- far distance, middle distance and near.
It is important for some people to be able to focus clearly at mid-range between distance and near. For example, Musicians may need to see their instruments close-up and read music at arm’s length while still being able to see the conductor in the distance. Someone with these needs will require trifocals, which give clear vision at three distances- far distance, middle distance and near.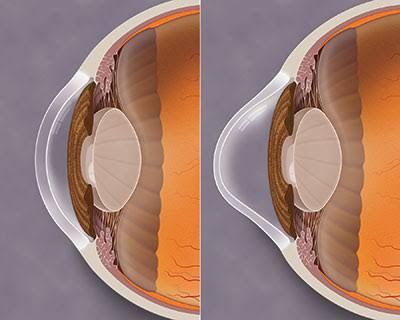

 The initial symptom of keratoconus is blurred vision, which is caused by shortsightedness and astigmatism. At this stage, good vision generally can be obtained with spectacles. As keratoconus progresses, the shape of the cornea becomes irregular and it is not possible to correct the vision with spectacles alone. We fit rigid contact lenses and scleral contact lenses to provide good vision. The contact lenses essentially provide a new, regular front surface for the eye, eliminating the distortions caused by the keratoconus. Because the cornea continues to change shape, it is important that people with Keratoconus have regular examinations to ensure that their contact lenses fit correctly. A poorly fitting contact lens can cause abrasions and scarring.
The initial symptom of keratoconus is blurred vision, which is caused by shortsightedness and astigmatism. At this stage, good vision generally can be obtained with spectacles. As keratoconus progresses, the shape of the cornea becomes irregular and it is not possible to correct the vision with spectacles alone. We fit rigid contact lenses and scleral contact lenses to provide good vision. The contact lenses essentially provide a new, regular front surface for the eye, eliminating the distortions caused by the keratoconus. Because the cornea continues to change shape, it is important that people with Keratoconus have regular examinations to ensure that their contact lenses fit correctly. A poorly fitting contact lens can cause abrasions and scarring.


 Presbyopia is usually first noticed around the age of 40 to 45 years. Although difficulties with close work may seem to come on suddenly, the aging process that causes presbyopia is gradual and has been going on since childhood. Between the ages of 45 and 65, the amount of presbyopia increases, making near work more difficult.
Presbyopia is usually first noticed around the age of 40 to 45 years. Although difficulties with close work may seem to come on suddenly, the aging process that causes presbyopia is gradual and has been going on since childhood. Between the ages of 45 and 65, the amount of presbyopia increases, making near work more difficult.